Download print version:
On this page:
- Statement of Acknowledgement for Aboriginal Peoples
- Statement of Inclusion
- A note from the artist
- Background
- Definition of clinical governance
- Purpose of this framework
- Pillars of Clinical Governance
- Roles and Responsibilities
- Pillars, Actions and Outcomes
- Pillar 1 - Leadership and Culture
- Pillar 2 - Child and family partnerships
- Pillar 3 - Risk management
- Pillar 4 - Monitoring, evaluating and reporting
- Pillar 5 - Clinical Practice
- Appendix 1 - Legislation and Policy Compliance
- Appendix 2 - References
- Appendix 3 - Supporting documentation
Statement of Acknowledgement for Aboriginal Peoples
We respectfully acknowledge the Aboriginal peoples as traditional owners of the land on which we live and work across South Australia, we acknowledge the continued cultural and spiritual connection that Aboriginal and Torres Strait Islander peoples have with country and waters. We respectfully acknowledge Aboriginal and Torres Strait Islander people as two unique and diverse peoples with their own rich and distinct cultures. We pay our respects to Elders past and present as well as emerging leaders who walk together in partnership on this journey.
We acknowledge the impact of historical policies that were harmful and have contributed to intergenerational trauma. This includes policies and practices of colonisation that have had a profound impact on Aboriginal and Torres Strait Islander people’s connection to country, culture and one another. We aim to continue to work together to promote self-determination, choice and healing while valuing Aboriginal and Torres Strait Islander people as strong, resilient people and decision makers in their own lives.
Statement of Inclusion
Safer Family Services (SFS) acknowledges and respects the UN Convention of the Rights of the Child (UNICEF 1989 The Convention on the Rights of the child) and upholds children’s rights by locating them at the centre of our work. At all times in the delivery of services, SFS will seek to advocate for a just and inclusive society that values and respects children’s identity and voice, within the context of their family, culture and community.
SFS staff and leaders create, model and promote a workplace culture where difference, lived experience, culture, gender identities, sexualities, faiths, ethnicities and abilities are respected and valued, and their voices elevated. We recognise the contributions these communities make and are committed to working alongside them in partnership (Odyssey House 2022).
SFS will address individual and systemic issues by tackling barriers or highlighting service gaps that prevent children from living safely with their families.
A note from the artist
The Child and Family Support system (CFSS) artwork is a visual representation of the ‘Aboriginal Cultural Lenses of Practice’. An appendix to the Aboriginal Cultural Practice Framework and reflects artwork correlating to cultural lens journey, allies walking alongside Aboriginal staff, families and communities and meeting and learning places supporting Aboriginal best practice.
The artwork came from the ‘Aboriginal Cultural Lenses of Practice’ Aboriginal led workshop attended by SFS Aboriginal staff and allies to give voice to Aboriginal ways of knowing, being and doing and guidance in the supporting of a culturally safe workforce. The artwork by Yamatji/Noongar woman Sasha Houthuysen/Hill is the representation of this voice and strength of culture. By using and engaging with these visuals it is a commitment made by Safer Family Services (SFS) to use a healing approach and ensure that children and families are front and centre and were working in culturally responsive and safe ways.
What we value
The symbol for what we value is the meeting place with people surrounding. This is reflective of the deep listening to all Aboriginal voices from all levels of the kinship system. This symbol represents Aboriginality as a protective factor.
What we want: now and into the future
The arrows reflect the risk and safety space we work in. The strength of this symbol is the understanding that high risk and safety concerns are present however they fall into the concentric circle representing family this shows that we aim to support families and communities to keep children safe and well at home.
Cultural strengths and responsibilities

Represents the journey that everybody takes which must be acknowledged and accepted, and especially the journey we wish allies to be on. This symbol also speaks to the cultural lens that needs to encompass our work with Aboriginal families.
A culturally capable workforce

Workforce needs is deeply rooted in cultural respect and the ability to walk the path together and build a relationship. This also speaks to the understanding that allies will actively walk this path committing to confront racist practices, structural racism and inequalities.
Cultural knowledge

Bright sparks show the strength and resilience of Aboriginal peoples and especially our Aboriginal workforce. This strength and resilience comes from a continual spark of motivation to work for and with our community to incorporate Aboriginal ways of doing, being and knowing into our practice.
The role of Allies

The symbol for role of allies is the journey line coming into a meeting place that is surrounded by Aboriginal people, this shows the various journeys people go on in their allyship and the importance of cultural lens application, meaningful consultation, and genuine partnership.
Background
In 2019, the South Australian Government released Safe and Well: Supporting families, protecting children (DHS 2020, Safe and Well, p.6). Safe and Well outlines a whole-of-government approach to reform South Australia’s child protection system, with a focus on three areas:
- Supporting: Provision of earlier, intensive, targeted support to families with multiple and complex needs to reduce incidents of child abuse and neglect and prevent children entering the child protection system.
- Protecting: Protecting children from harm, including when they enter care. Delivery of trauma responsive, developmentally appropriate services, designed to meet the individual needs of children and young people in care with an emphasis on family-based care, reunification and permanency.
- Investing: Investing in children and young people in care and their transition from care. To support them to acquire life skills and to help to break intergenerational contact with the child protection system.
The Department of Human Services (DHS) leads the Supporting focus area of the strategy and funds and delivers a range of services within it. At the leading edge of this reform is the Roadmap for reforming the Child and Family Support System 2021–2023 (DHS 2020, Roadmap for reform). The Roadmap provided the blueprint for the Child and Family Support System (CFSS) in the creation of support services for children and families with complex needs, that is evidence based, culturally responsive and trauma informed. Services are designed to increase the likelihood that children are safe and well in families, community and culture and by improving outcomes for children and families, avoid the need for the involvement of tertiary child protection services.
The system is led by the voices, perspectives and aspirations of Aboriginal peoples in order to create a system that will work for Aboriginal and Torres Strait Islander people. The CFSS Aboriginal and Torres Strait Islander System Design criteria and Co-Design principles were implemented (DHS 2019, Co-design Report) and the co-design process draws upon knowledge from those with lived experience and those who deliver services, as well as findings from data and research.
Definition of clinical governance
Clinical governance is defined as ‘…the system by which the governing body, managers, clinicians and staff share responsibility and accountability for the quality of care, for continuously improving, minimising risks and fostering an environment of excellence for users of the service (ACQSC, 2019)’. The components or pillars of clinical governance, and the focus and scope of these components can vary, depending on the clinical or community setting.
Purpose of this framework
The purpose of the SFS Clinical Governance Framework (CGF) is to ensure the quality, safety and accountability of clinical services provided through SFS programs, to infants, children, young people and their families. The CGF outlines the supports provided to the workforce in relation to managing safety, complexity and risk while working with families to meet the needs of their unborn children, infants and young people.
Managing risk is at the heart of social work practice, and informed and committed social workers are the most important resource in implementing risk management successfully (Hardy, R. 2017). The framework outlines the critical roles and responsibilities of SFS practitioners and leaders in relation to risk management and the timely escalation of risk, and demonstrates the embedded nature of risk management, within and across clinical governance activities.
The framework sits alongside other key documents that form the foundation of the work and that guide clinical practice and system design. These are the Aboriginal Cultural Practice Framework (DHS 2022, Aboriginal Cultural Practice Framework), the Trauma Responsive System Framework (DHS, Connected Self, 2022 Trauma Responsive System Framework), the Case Management Framework (DHS 2020 Case Management Framework) and the CFSS program level outcomes hierarchy (DHS 2020 Building a Coordinated Child and Family Self Learning System). It is also of great importance in this work to understand, adhere to and embed the Aboriginal and Torres Strait Islander Child Placement Principles (ATSICPP) (SNAICC 2013 Aboriginal and Torres Strait Islander Child Placement Principles) in their entirety because knowledge of a child’s identity will inform how practitioners work with the child and their family across all phases of child safety and wellbeing.
The clinical governance framework provides guidance for the delivery of and continuous improvement in culturally safe, trauma informed and high-quality clinical services. These services are provided as part of a holistic approach, based upon the needs and goals of children and their families, with an explicit focus on keeping children safe within their families, community and culture.
The framework outlines the five interlinked components (or pillars) that are integral to building service excellence within SFS. The pursuit of quality is the driving force behind governance arrangements. Success in delivering high-quality child-focussed services requires the involvement and engagement of all levels of the workforce, from frontline staff through to administrative support, supervisors, managers and the executive (Scottish Government, 2015) (Victorian State Government, 2018).The clinical governance framework describes the systems, structures, processes and roles and responsibilities that enable all of organisational accountability, for the delivery of child-focussed, safe and high-quality services (Wentworth Healthcare, 2019).
Service Principles
Safety is unique to each child, young person or family.
The CFSS delivers services that are based upon the overarching government and public sector policies, values and codes of conduct and on the four core principles of the United Nations Convention of the Rights of Child (UNICEF 1989, Convention on the Rights of the Child). When implemented, these principles allow for both the wishes of the child to be heard while still guaranteeing them necessary protection (ibid). The four principles are: non-discrimination, the best interest of the child, the right to life, survival and development and respect for the views of the child (ibid).
In terms of SFS practice with families, this translates to:
- respecting, building trust and preserving family by keeping children safe at home, supporting their unique connection to culture, with practitioners utilising an empowering and trauma informed, healing approach
- children’s rights, safety, identity and voice are at the centre of service provision
- risk is acknowledged, managed, and escalated where necessary
- working in collaboration, sharing knowledge and growing active partnerships
- a culture of learning, that values courage, reflection and evidence informed practice
Safety encompasses strengths and protective factors that can be drawn from and worked towards, to create physical, emotional, sexual, environmental, cultural and spiritual safety. The CFSS recognises safety as more than the absence of harm and exposure to risk. The CFSS is committed to keeping children and young people safe and well at home, with a sense of belonging and identity in family, community and culture (DHS, 2022 Common Elements).
Pillars of Clinical Governance
The SFS Clinical Governance Framework is comprised of five integrated key components or pillars, that have as their foundation, trauma informed and culturally responsive practice approaches and principles, which are reflected and implemented at all levels of the service system (diagram on page 8).
The framework outlines action to support good clinical outcomes across levels of the organisation by:
- setting the strategic direction for clinical quality and safety
- referring to the organisational structure, policies and procedures that operationalise the strategic direction
- describing the roles and responsibilities of those in the organisation who are responsible for implementing the strategic direction and providing and overseeing the delivery of services and systems improvement (Wentworth Healthcare 2019, p.3)
Supporting the framework are policies, procedures and practice guides that provide further details about specific strategies, processes and activities to support safe, high-quality client care.
The framework is designed to allow practitioners, supervisors and leaders to:
- establish and review roles, responsibilities and accountabilities
- ensure the conditions (organisational environment, leadership, and professional support) are in place to promote practitioner capability and wellbeing
- create awareness of how clinical governance systems effectively monitor risk and risk management
- take responsibility for their own practice, learning and development (ibid)
- interact with other frameworks such as the Aboriginal Cultural Practice Framework, to explicitly align clinical and cultural practice.
The Safe and Well Diagram
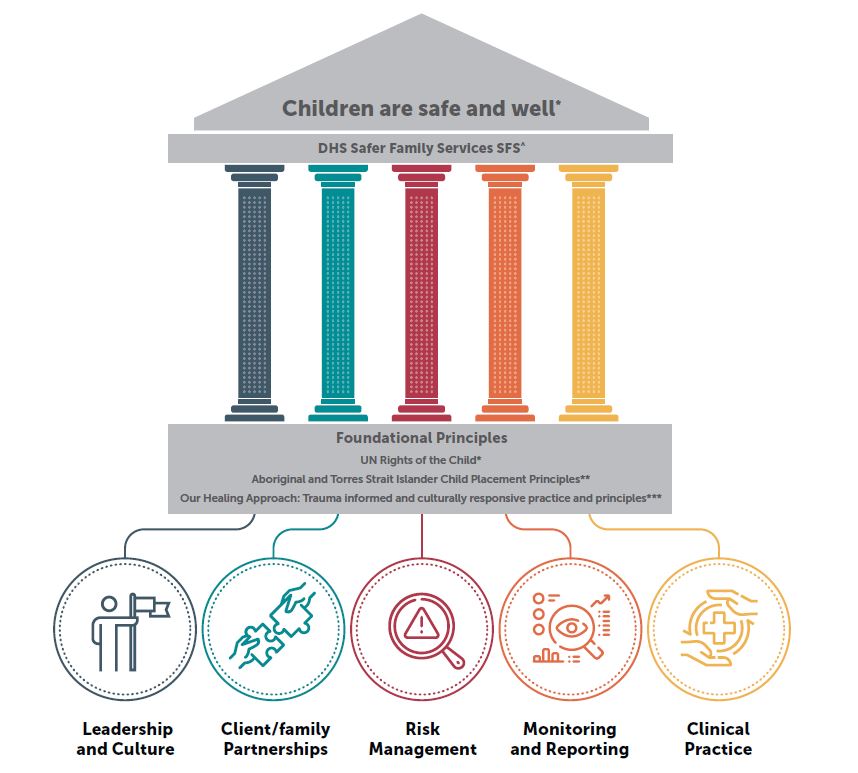
The Safe and Well diagram in plain text
Roles and Responsibilities
The delivery of high-quality services and outcomes for children and families is reliant on all staff in the organisation playing a role. Distinguishing roles and responsibilities within a clinical governance framework is critical to ensure effective implementation of clinical activities. All staff, from practitioners to executive should focus on (Headspace, 2014, Clinical Governance Framework):
- partnering with children, families, and communities
- establishing and maintaining a culture of risk awareness
- regular review, evaluation, and identification of areas for improvement
- ownership and accountability for the quality of services provided (Victorian Government 2018 (p14))
The safety and wellbeing of children is central to our work in supporting children and the adults who care for them. Their experiences of and participation in services are fundamental indicators of quality and safety. Children and families:
- participate to their desired extent and ability in the services they receive, in full knowledge of the options and potential outcomes related to their choices
- participate in system wide service improvement
- share their experience, provide feedback, and offer suggestions to support service improvement
Throughout this process, practitioners will ensure that:
- children are seen, heard and listened to, resulting in meaningful action to support safety
- children and families have access to non-judgemental, trauma informed and culturally responsive services that consider their unique circumstances
- children and families are encouraged to engage, lead, advocate and make decisions that best support children’s safety
- family led decision making is a priority
- they work within the scope of their role and recognise and act on their responsibility to escalate risk
- children and families are encouraged and supported to provide feedback, offer suggestions and will receive feedback about their contribution
- SFS staff are compliant with and accredited in, mandatory training obligations and actively accountable to their Aboriginal cultural learning journey
Front line practitioners are uniquely positioned as the “face” of SFS and of service quality.
Practitioners are responsible for:
- promoting and role modelling cultural safety and recognising the strength of culture by supporting Aboriginal Family Led Decision Making, Aboriginal parenting practices and client self determination
- their own journey toward allyship accountability
- raising any safety concerns for children and families in honest, sensitive and non-judgemental conversations with families. Being honest around potential outcomes related to the choices that the family makes
- awareness of their responsibility to work within the scope of their role and to escalate heightened risk
- following protocols in relation to risk and risk management
- respectfully, actively and with curiosity, engaging with children and their families
- working collaboratively with children, families, community, peers and partner agencies
- raising any safety concerns for themselves or colleagues with supervisors
- working from a trauma informed approach
- seeking cultural consultation as required
- appropriately accessing and using information
- sharing information respectfully, sensitively and in culturally appropriate ways to further the best interests of the child, family and community to increase safety or provide services
- performing functions and fulfilling roles within the context of legislation, professional ethics, public sector and agency standards and guidelines
- consulting and seeking case plan endorsement from their supervisor
- actively engaging in reflective practice opportunities including clinical supervision, cultural supervision, and professional development opportunities
- ensuring timely, accurate and up to date case records, data and reporting requirements.
Supervisors are responsible for:
- promoting and role modelling cultural safety and recognising the strength of culture by supporting Aboriginal Family Led Decision Making, Aboriginal parenting practices and Aboriginal self determination
- supporting cultural supervision, including strengthening their own journey towards allyship accountability
- working from a trauma informed approach
- establishing and maintaining a culture of risk awareness
- identifying and managing situations of elevated risk and understanding their individual role in the safety, quality and risk management processes
- providing a safe workplace for supervisees and teams that supports collaboration, teamwork and transparency
- performing functions and fulfilling roles within the context of legislation, professional ethics, Public Sector and agency standards and guidelines
- being visible, accessible, and responsive and applying informed decision making based on evidence, consultation and best practice
- providing effective clinical supervision that is documented and per the SFS Clinical Supervision Practice Guide that includes authorising and endorsing case direction
- actively engaging in reflective practice opportunities including supervision of their clinical supervision and professional development opportunities
- promoting a culture of continuous improvement and supporting practitioners to contribute to and lead improvement efforts
- communicating service delivery challenges or opportunities to leadership and advocating for resources to support service delivery.
Leadership are responsible for:
- promoting and role modelling cultural safety and recognising the strength of culture by supporting Aboriginal Family Led Decision Making, Aboriginal parenting practices and Aboriginal self determination
- being responsible for their own journey towards allyship accountability
- working from a trauma informed approach
- providing visible leadership and a commitment to delivering the organisations strategic objectives
- supporting supervisors with risk, risk management and escalation processes as per agency policy
- ensuring governance mechanisms effectively monitor risks and the way in which they are managed
- being visible, accessible and responsive to the needs of supervisors and their teams
- advocating for service improvements and embedding approaches that promote cultural safety for clients and staff
- empowering staff and providing a safe environment that allows for diversity of view, encourages staff to speak up and supports robust discussion that is solution focussed
- ensuring clinical supervision occurs within teams in accordance with SFS clinical supervision practice guidance
- translating and communicating clinical governance strategy and policy at program and service level
- actively engaging in reducing systemic barriers that impact front line staff delivering services to children and families
- leading improvements, engaging and identifying opportunities to incorporate client and practitioner experiences and expertise in systems change
- maintaining a culture of continuous improvement, advocating for service improvement and representing practitioners at the corporate level if adverse or critical events occur.
Director is responsible for:
- promoting and role modelling cultural safety and recognising strength of culture through continued organisational emphasis on supporting Aboriginal protocols and parenting practices, as well as Aboriginal self determination
- being responsible for their own journey toward allyship accountability
- working from a trauma informed approach
- providing visible leadership that promotes an open culture and commitment to continuous improvement, that prioritises and supports service delivery and standards of care consistent with vision of DHS, SFS and broader CFSS sector
- demonstrating an understanding of and commitment to an integrated risk management system
- supporting service delivery by timely, clear and decisive decisions on critical matters
- providing leadership that commits to fairness, transparency, openness, learning and improvement opportunities that empowers staff to raise quality and safety concerns
- providing role clarity, tools resources and opportunities at each level of the organisation to support staff to deliver best possible services to children, young people, and their families
- overseeing improvements, strive for excellence, and drive a culture that is committed to listen to the voice of children and their families in service improvement
- proactively seeking the evidence that informs future developments.
Executive Director is responsible for:
- setting a clear vision and strategic direction that is reflected in SFS clinical and cultural governance framework and Safe and Well roadmap
- implementing strategic documents and direction
- being responsible for their own journey toward allyship accountability
- providing visible leadership with a commitment to SFS programs and priority populations
- ensuring they are regularly briefed on quality, safety and risk in all areas of operation
- setting an organisational culture that drives consistently high-quality services and facilitates employee engagement
- committing to transparency and system reform by seeking information from SFS executives, leaders, staff and priority populations and utilising information for system and resource advocacy and improvement.
Pillars, Actions and Outcomes
(Table adapted from: ACQSC 2019, Radovini 2014, WA Government 2018, Practice Governance Group Scotland 2015, State Services Authority 2013, Victorian Government 2018)
The following tables demonstrate how the pillars or the components of clinical governance and the roles and responsibilities previously outlined, are operationalised in SFS. It also demonstrates the outcomes (or measures of success) of effective implementation of roles and responsibilities at differing levels of the organisation.
Pillar 1 - Leadership and Culture
Leaders are actively engaged in leading and supporting the provision of services to promote safe, quality care and facilitating a culture of transparency, accountability, allyship and teamwork. Pillar 1 originated from the West Australian Government, 2018, Clinical Governance Framework.
Actions
- Leaders are committed in their personal and professional journey towards allyship accountability and demonstrate this through modelling, promoting and actively engaging in allyship learnings through reflective practice and activities.
- Staff participate in meaningful cultural activities, acknowledge significant dates and understand and actively engage in reflective practice about Aboriginal ways of knowing, being and doing
- Leaders and practitioners utilise a trauma informed approach.
- Leaders embrace and model a culture within SFS of diversity, inclusion and respect, with reciprocal communication and feedback across the organisation
- All staff work within a culturally safe organisation, where families, staff and community can be authentic and freely without fear of discrimination or repercussion express their voice, identity, and culture.
- Leaders will model collaborative ways of working, support teamwork and transparency
- All staff will work towards full implementation of DHS Diversity and Inclusion Strategy
- Practitioners and staff utilise opportunities for feedback (supervision, consultations, Teamgage and other surveys) as well as participate in service development initiatives (DHS, 2021-2023, Diversity and Inclusion Strategy).
- Statements of Inclusion are visible and respectfully implemented.
- Leaders support the empowerment and development of practitioners, so they can act more autonomously, confidently and skilfully - in order to shift power and control to the families they support. Leaders have a role in creating an organisational culture that supports this approach
- Practitioners make well informed decisions using professional judgement, best practice approaches and creativity, within a framework of accountability.
- Policies and procedures are in place to facilitate practitioners to practice safely and creatively.
- Practice is openly reviewed when things go well or go wrong with a no blame culture and learning is shared.
- Aboriginal families are given choices to actively create meaningful self-determination through culturally responsive practices.
- Leaders demonstrate leadership and foster a culture of openness, partnership, learning and continuous improvement
- Leaders identify, articulate, and model the values, norms and ways of interacting within and across SFS.
- Practitioners adopt behavioural norms and maintain acceptable standards of work that align with organisational values.
- Leaders are visible, accessible and available
- Leaders and practitioners are engaged in learning and development, linked to organisational and individual priorities and objectives to support ongoing service improvement.
- Leaders build an open culture based on consistent clinical quality and safety and integrate clinical governance into organisational governance. Leaders and managers communicate and operationalise clinical governance strategy and policies at the program level
- Management and executive are informed of and understand clinical issues.
- Leaders are aware of how clinical governance impacts upon and is impacted by other aspects of governance such as risk, financial and human resources
- Practitioners have role clarity, skills and training to provide safe, high-quality services to families that is evidence informed, and adheres to legal, ethical and policy requirements (Delaney, L., J., 2015).
- Practitioners and staff receive regular communication of priorities and are aware of new and existing policies and standards.
- Leaders are of the belief that cultural practices and governance are heavily embedded in clinical and organisation governance.
- Provision of effective, supportive, reflective and regular clinical supervision
- All frontline staff have supervision agreements and participate in regular supervision that includes review of workload capacity, practitioner wellbeing and best practice requirements.
- Supervision is a reflective process that supports professional social work practice, sound clinical judgement and continuous professional development
- The supervision process will also consider risk, risk levels and risk management within practitioner caseloads
- Clinical supervision will ensure a cultural lens application.
- Leaders are able to identify, understand and support the management of risk, with clear lines of responsibility for leading the escalation of issues and the escalation process.
- Practitioners understand and work with risk, confident that there are processes and procedures in place to support them to work with and manage risk, as well as understand and access the escalation process
- Practitioners understand and adhere to their responsibility to escalate heightened risk
- Leaders ensure that practitioners and supervisors receive support in fulfilling their responsibilities, related to the management and escalation of risk
- The role of Practice Leads and High Risk alerts is understood as they relate to risk management
- Practitioners are of the belief that Aboriginality is not an inherent risk factor.
Pillar 2 - Child and family partnerships
Children are at the centre of service responses. Systems are designed and used to support families to be partners in service planning and delivery, and inform evaluation and ongoing quality improvement
Actions
- Children and families actively engage and direct (to their desired extent and capacity) decision making to plan for safety and their service journey
- Families are engaged and working towards the safety and wellbeing of their children and measurable and lasting change within the family.
- Families are informed of and understand the potential consequences of their decisions around engagement and participation.
- Service provision is premised upon trauma informed and culturally responsive practice approaches that utilise a healing approach
- Practitioners understand and actively implement CFSS Trauma Informed System Framework
- Practitioners understand and actively implement SFS Aboriginal Cultural Practice Framework and adhere to the Aboriginal and Torres Strait Islander Child Placement Principles.
- Families are made aware of their rights; consent is sought and meaningful engagement with families is a priority
- Clear, honest and respectful communication exists between staff, children, families, kinship networks, CFSS partners and other agencies-resulting in connected, inclusive and culturally responsive service provision to families.
- Children and families feel that their practitioner and care team is honest with them and is walking alongside them in their healing journey.
- SFS work to provide a connected service system experience for children and families, with strong partnerships across CFSS
- Leaders and practitioners work towards creating meaningful engagement. Data on individual and local needs as well as data from partner agencies, is integrated into service improvement planning and activities.
- Service design, planning and monitoring are informed by feedback from children and families and partner agencies
- Children and families feel supported, safe and heard and have an active voice.
- SFS collaborate with external agencies and the child and family in an iterative process to shape services and secure outcomes in the interest of the child and family.
- Children and families understand their rights and are aware of feedback processes. Complaints are acknowledged, appropriately responded to and feedback provided to all parties involved
- Lived Experiences and Aboriginal voices shape system design.
- Restorative justice principles are used to ensure that individuals, families, services and agencies are able to proactively build relationships and avoid or resolve conflict (Australian Association for Restorative Justice)
- Practitioners will hold the safety of children as paramount and their voices will be prioritised.
- Practitioners will hold the child and family as expert, with a response that considers the role of family and community supports
- Family Group Conferencing, Family Led Decision Making practices and elements of the Aboriginal and Torres Strait Islander Child Placement Principles will be utilised.
- Services and information are accessible to all children and families
- Families are offered cultural supports, translators or translated information where required
- Disability needs are considered and attended to when engaging and working with children and families.
Pillar 3 - Risk management
There is a structured approach to assessing, managing, and working with risk that draws on evidence-based approaches and is supported by robust risk management systems and escalation processes
Actions
- Leaders and practitioners adhere to the policy and legislative context of SFS and the identification and proactive management of incidents, escalation and risk.
- Leaders establish and maintain a culture of risk awareness
- Leaders and practitioners actively support, report on and contribute to the risk management process
- Risk is acknowledged and managed coherently in line with policy, legal and ethical obligations.
- Systems are in place to identify, prioritise, manage and escalate risks.
- Practitioners are aware of their responsibility to communicate and escalate risk, in a timely manner.
- Leaders understand risk and respond to escalations in a timely and appropriate manner
- SFS are part of a service system that collectively holds risk with partner agencies
- Leaders and practitioners work in partnership with children, their families, community and with partner agencies to create safety and acknowledge, mitigate or manage and address shared risk.
- Policies and procedures exist to manage inherent risk and provide processes for escalation of risk or safety, where required
- SFS recognise that risk management is a dynamic and evolving process that is responsive to change
- Policy and procedures for risk management and escalation are based on evidence and best practice and are reviewed and updated as needed (Refer to appendix for legislation and policy, and SFS procedures and resources to manage risk)
- Practitioners understand and act on their responsibility to work within the scope of their role and to escalate heightened risk
- Leaders and practitioners are aware of and understand the policies, procedures and systems in place and use them to inform and guide safe, high-quality services to children and families
- Leaders are familiar with Root Cause Analysis (RCA) and utilise RCA principles to identify contributory systems issues for critical incidents and recommendations for preventing or minimising their recurrence
- Leaders and practitioners are aware of their statutory obligations related to managing risk, such as the role of SAPOL, mandatory reporting, FOI legislation, use of Information Sharing Guidelines and organisational reporting requirements.
- Processes are in place to address ethical decision making and conflict of interests, system advocacy and resource allocation
- Formal clinical supervision is a forum for reflection on effective and ethical practice
- Cultural and clinical practice will align and not be competing practices
- Practitioners and supervisors recognise that risk cannot be eliminated. Clinical supervision is a forum for critical reflection on balancing ethical issues and best outcomes for clients, with sound risk management practices
- Leaders and practitioners are familiar with principles of duty of care as well as Public Sector/Australian Association of Social Workers (AASW) Codes of Conduct and Ethics
- Practitioners will work within the scope of their role and consult where required
- SFS/DHS Policies exist for management of conflict of interest (See appendix 3 - supporting documents).
- DHS Risk Management, reporting tools and HR processes are used, where required
- Staff are trained in the SA Government hazard and incident reporting system.
- Staff are aware of their Wellbeing and Safety obligations related to workplace safety.
- Systemic or workplace issues are escalated to leadership and/or HR to prioritise, support and facilitate system improvement responses
- DHS/SFS guidelines for home visiting in COVID or other pandemic are followed.
- Worker screening, in line with legislation and agency requirements
- All staff have current Working with Children check
- All frontline staff will have current child safe accreditation.
- Processes are in place to monitor currency of screening and compliance.
- Risk to workers undertaking home visits is minimised
- Practitioners utilise safe work practices and comply with policy to mitigate risks of home visiting (See appendix 3- supporting documents).
- Practitioners follow DHS/SFS guidelines on home visiting and workplace processes in pandemic situations (See appendix 3 - supporting documents).
Pillar 4 - Monitoring, evaluating and reporting
Safety and quality systems are integrated with governance processes to monitor and improve the quality of services provided to families
Actions
- Child and family, SFS workforce, CFSS partners and other agency feedback is incorporated within system improvement processes
- Feedback from Lived Experience network (LEN), from families, service partners and Aboriginal voices is prioritised and is incorporated in policy development and practice guidance.
- Practitioners comply with system and program data collection in a timely manner, as per practice guidance
- SFS incorporates risk management into business planning and is informed by data collection from SFS workforce, agency partners and clients and tailored to meet SFS needs
- Feedback from Teamgage is incorporated into organisational team building and development
- Children, families, CFSS partners and other agencies have access to and are aware of complaints reporting and feedback processes.
- Leaders, supervisors and practitioners are committed to reviewing and reflecting upon their performance, and their contribution to continuous improvement and organisational outcomes
- All staff are aware of DHS and SFS strategic priorities and comply with practice standards
- All practitioners and supervisors participate in clinical supervision, cultural consultation, case reviews and case conferences
- All staff participate in bi-annual Performance Development Plan meetings
- Practitioners are familiar with and work toward meeting SFS KPI’s. KPIs are aligned to DHS and SFS strategic priorities
- Professional development is prioritised and tailored to the work
- Mandatory training is completed.
- Supervisors monitor the quality, safety and efficacy of clinical case work through clinical supervision (including review of case notes, assessment and case management documentation) in accordance with legislation, best practice for client outcomes, culturally responsive practice, trauma informed practice and quality improvement
- Client records demonstrate clinical quality and provide accountability in service provision
- Record keeping is in accordance with legislation and SA Government State Records Act (1997).
- Case records provide a clear outline of interventions, actions and outcomes, risk and escalation, where indicated
- Case records demonstrate use of culturally responsive, trauma informed and strengths-based approaches in clinical casework
- Case records are completed in a timely way, are objective, concise, clear and non-judgemental.
- Effective monitoring of service demand, performance, outputs and outcomes with comparative analysis to best practice nationally and internationally
- CFSS and EIRD work together to ensure data analysis is shared and applied to SFS program design.
- Practitioners utilise information from data to inform service provision
- Leaders and practitioners strive toward continuous improvement that is driven by feedback from practice, data analysis, best practice approaches and organisational need.
- Executives and managers review information on clinical quality and safety performance as part of a continuous quality improvement approach for the workforce
- Incidents are acknowledged, reported and analysed. Findings are used to improve the service system
- SFS is responsive to identified practitioner training requirements and practice needs, providing adequate resourcing to support organisational outcomes.
- Appropriate and timely sharing of information between providers, where necessary to address risk and increase safety
- Practitioners and leaders are familiar with and utilising appropriate information sharing legislation and protocols (FOI, ISG, client consent).
- Practitioners are responsible for adhering to codes of practice and for managing professional development needs
- Clinical practice is ethics based and practitioners are adequately skilled and trained to undertake the work.
- Practitioners are responsible for identifying gaps in their knowledge and undertaking related training needs
- Practitioners commit to allyship accountability and both a professional and personal cultural learning journey.
Pillar 5 - Clinical Practice
The workforce has the right information, skills and supervision to provide safe, high-quality services to children and families.
Actions
- SFS work within the context of the child and family’s cultural identity, ensuring services are culturally responsive, safe and consider an intersectional approach (Recognition that children, young people, and their families may experience multiple and intersecting systemic barriers or discrimination due to their unique intersection of identities and situation)
- Clinical practice is supportive, nurturing and respectful- committed to truth telling and is culturally safe.
- Clinical practice is informed by an awareness of power dynamics and how this impacts intersectionality and diversity
- When cultural and clinical practice align, strength and safety occur in the wholeness of family, community, identity and culture
- The Aboriginal and Torres Strait Islander child placement principles and precursor of identification will be adhered to in its entirety.
- All staff will intentionally work from a healing and trauma responsive approach
- Practitioners actively embed Our Healing Approach, utilising the Common Elements Practice Guides and SFS practice guides to support trauma responsive practice
- Practitioners will adhere to the Trauma Responsive Framework.
- SFS staff embrace allyship by aligning values and actions in support of, acknowledgement and respect for Aboriginal and Torres Strait Islander peoples and diverse cultures
- Practitioners report they are well supported to understand their role as allies and how this forms part of trauma responsive practice
- SFS is a supportive, safe, nurturing and positive environment that is culturally responsive and enriching. Families, staff and community can be authentic and express their voice, identity and culture through Aboriginal ways of knowing, being and doing without fear of discrimination and repercussion
- Practitioners commit to allyship accountability and both a professional and personal cultural learning journey.
- Practitioners work with UN Conventions of the rights of children- as front and centre of the work
- Children’s safety, rights and voice are prioritised in all work with families
- Child safety is paramount.
- Front line staff assess levels of risk, develop safety plans, provide relational case management, connect families to support services and take a lead role in delivering and coordinating multi agency responses
- Families receive high quality case management services that have a focus on the safety of children within family, community and culture.
- Practitioners consult on issues of cultural or ethical complexity, conflicts of interest and instances that may require escalation.
- Practitioners are familiar with and effective in relational and strengths based case management approaches.
- SFS has effective relationships with external agencies and health providers
- Existence of partnering agreements with service partners including shared outcomes
- Supervisors attend interagency meetings and forums
- Collaborative co-working occurs across systems levels
- DHS Aboriginal Workforce Strategy (2021-2023) is upheld and cultural safety and retention is paramount
- Practitioners commit to allyship accountability and both a professional and personal cultural learning journey.
- SFS takes a strategic approach to the recruitment, training and ongoing development of the workforce that ensures the provision of safe, quality clinical services to children and families
- HR/recruitment processes consider the alignment of data on client need with worker skills.
- Induction programs, organisational frameworks, practice tools and guides and strategic plans are utilised to upskill and orient both new and existing staff.
- Appropriate training is prioritised.
- Productive links are formed between individual learning, PDP’s, service development and organisational goals.
- Clinical delegations are clear and understood, and outlined in the Clinical Supervision Practice Guide
- All staff are familiar with and undertaking their obligations related to clinical supervision, as outlined in the Clinical Supervision Practice Guide
- Clinical supervision will reflect a cultural lens.
- Practitioners and supervisors are clear in relation to their role and responsibility relating to clinical supervision, as well as that of their supervisor and the organisation.
- All practitioners participate in clinical supervision that is reflective, critically evaluates their practice and supports ongoing learning, critical reflection and improvement
- Supervisors provide effective supervision and support case management direction and decision making
- Processes for consulting with the Clinical Practice Team and Cultural consultants are known to practitioners.
- Key legislation is understood and complied with
- Obligations under the Child and Young People (Safety) Act 2017 are understood. Practitioners make CARL notifications when there is suspicion of harm and record on C3MS in a concise, accurate and timely way
- Case note recording on C3MS is timely, accurate, objective and concise and in accordance with Clinical Case Noting Practice Guide
- Practitioners are aware of FOI legislation, ISG legislation and other state Acts and legislature that have relevance to their work.
Appendix 1 - Legislation and Policy Compliance
Commonwealth Legislation
Disability Discrimination Act 1992
Equal Employment Opportunity (Commonwealth Authorities) Act 1987
State Legislation
Children and Young People (Safety) Act 2017
Child Safety (Prohibited Persons) Act 2016
DHS Diversity and Inclusion Strategy 2022–2023 A workplace where we can all thrive
Family and Community Services Act 1972
Freedom of Information Act 1991
Health and Community Services Complaints Act 2004
Independent Commissioner Against Corruption Act 2012
Intervention Orders (Prevention of Abuse) Act 2009
Public Finance and Audit Act 1987
Work, Health and Safety Act 2012
Youth Justice Administration Act 2016
Other requirements
Aboriginal and Torres Strait Islander Child Placement Principles (SNAICC)
Code of Ethics for the South Australian Public Sector
Committed to Safety: A Framework for Addressing Domestic, Family and Sexual Violence, March 2019
UN Convention on the Rights of the Child
Declaration of Principles Regarding the Treatment of Victims, Commissioner for Victims Rights
Family Group Conferencing – Courts Administration Authority
Information Sharing Guidelines for Promoting Safety and Wellbeing (ISG)
Interagency Code of Practice – Investigation of Suspected Child Abuse and Neglect
AASW Social Work Code of Ethics 2020 (PDF 251 KB)
Appendix 2 - References
Australian Association for Restorative Justice, Family, Victoria Online Resource
Australian Government, Canberra 2019. Aged Care Quality and Safety Commission, Core elements of clinical governance.
Australian Government, Canberra 2019. Aged Care Quality and Safety Commission, Developing and implementing a clinical governance framework.
Australian Government 2019 Wentworth Healthcare, Nepean Blue Mountains, Clinical Governance Framework.
Australian Human Rights Commission, 2018. Principles of child safe organisations. Online resource
Delaney, L. J.,2015, challenges of an integrated governance process in healthcare. Clinical Governance: An International Journal, Vol. 20 No.2,pp74–81. Online resource:
Government of South Australia, Department for Human Services,2021–2023 Aboriginal Workforce Strategy. Online resource
Government of South Australia, Department for Human Services, 2020, Building a Coordinated Self-Learning Child and Family System: the Outcomes Hierarchy Working Group review of outcomes measurement tools, August 2020. Online resource:
Government of South Australia, Department for Human Services, 2020, Case Management Framework. Online resource:
Government of South Australia, Department for Human Services, 2020, Co-design findings and next steps: Child and Family Support System June–October 2019
Government of South Australia, Department for Human Services, 2022, Aboriginal Cultural Practice Framework
Government of South Australia, Department for Human Services, , 2020, Diversity and Inclusion Strategy 2020–2023. Online resource:
Government of South Australia, Department for Human Services, 2022, Trauma Responsive System Framework Online resource
Government of South Australia, Department for Human Services, South Australia 2020 Safe and Well: Child and Family Support System Roadmap for Reform.
Government of South Australia, Department for Human Services 2022, Common Elements, Increasing safety through conversations
Hardy, R. 2013 Tips on managing risk in social work, Community Care Inform, UK. Online resource
Info.Diagram. Online resource 13 Corporate Strategy Pillars Graphic Charts PPT Template for Business Plans and Project Management Operations Presentation (infodiagram.com)
Radovini, S., 2014 Clinical Governance Framework, Headspace National Youth Mental Health Foundation. Australian Government Department of health and Ageing
Odyssey House 2022 Diversity and Inclusion Statement. Online resource
Scottish Government Scotland, Social Work Scotland., 2015. Governance for quality social care in Scotland (PDF 980 KB), Verity House, Edinburgh. Online resource
Secretariat National Aboriginal and Islander Child Care (SNAICC), 2013. Aboriginal and Torres strait Islander Child Placement Principle: Aims and Core Elements - Briefing Paper. Online resource
State Services Authority, 2013, Victorian Government. Organisational Culture. Online resource
The Scottish Government, Practice Governance Group, 2011. Practice Governance Framework: Responsibility and accountability in social work practice, Changing Lives. Online resource
UNICEF 1989 The Convention on the Rights of the child
Victorian Government, Health and Human Services 2018., Community services quality governance framework; safe, effective, connected and person centred community services for everybody, every time Online resource
West Australian Government, Department of Health, 2018 Clinical Governance, Safety and Quality. Online resource
Appendix 3 - Supporting documentation
DHS Safe and Well: Child and Family Support System Roadmap for Reform
DHS Trauma Responsive System Framework
SFS Case noting Practice Guide
SFS Risk and Escalations Practice Guide
SFS Safe Home Visiting Practice Guide
SNAAIC- The Aboriginal and Torres Strait Island Child Placement Principle
Documents for internal DHS use and accessed from the DHS Intranet
DHS intranet – People and Culture
SFS Clinical Supervision Practice Guide
SFS High Risk Alert Practice Guide

